[This isn’t a plea for more help. I try to spread my requests out, because everyone has their own lives. I have actually had certain friends get mad at me because I asked for help more than once in a year. So in the spirit of friendship no, I don’t need anyone to get my groceries or prescriptions.]
Facebook is great until it’s not. Just hang with me as I explain this.
I’ve got so many medical conditions, allergies, prescriptions, over-the-counter medications and supplements that I have everything alphabetized on a sheet that I keep updating and printing every time I go to appointments. I can’t remember everything. I’ve got two injections that I give myself every week in my stomach and thighs, and it’s possible I’ll be getting a third. One of them really hurts and it takes a long time to push the syringe down; my hands cramp up and a few times I didn’t go long enough and have shot the solution all over myself when I pulled the needle out. (I hate wasting that precious medication.)
Nothing is simple with my healthcare. I just got done coordinating a treatment for hidradenitis suppurativa, which means I have to fly to Minnesota for two different lasers and get Pronox gas since Lidocaine doesn’t work on me topically. One of the issues we had to figure out was what to do about me breathing back OUT into the air – what if I was breathing out contaminated microbes and spreading COVID-19? So the office had to track down a device to add to the machine. It took me a week and a half to put everything together and find flights/hotel that I could afford that would also work with the office’s schedule.
At the same time, I was also scheduling surgery for some scarred areas with the hidradenitis suppurativa. Again, since I don’t get numb from Lidocaine, I have to be put under completely to get the spots removed. They are not going to be closed up but rather left open because of the nature of the condition; it’s better not to make a tunnel, that would just encourage the disease to start again in those spots. So now I have to also reschedule other doctor appointments because I will be uncomfortable for a couple of weeks, especially since I can’t take pain medications because of mast cell activation syndrome.
I met with a new cardiologist because I’ve been having major problems with pitting edema, despite being on a very high dose of spironolactone. He put me through a very thorough ECG and ultrasound of my heart and carotid artery, and wants me to have a tilt table test performed. I have a resting heart rate of 110+ now but a very normal blood pressure which sometimes dips low and have had the diagnosis of POTS since 2017 (but symptoms since 2000), but he wants to be sure that that is what I’m still dealing with. When it gets into the summer months here in Phoenix, it gets a lot harder for me to deal with the heat, and I get closer to blacking out frequently, even in my apartment with air conditioning.
I saw my OB/GYN because I still have cysts in my breasts. I get checked every six months. So far they haven’t changed in size, so I might be able to go once a year.
I was being lectured by my primary care doctor and rheumatologist about being on steroids long term for ankylosing spondylitis. I told them that going off for even a day is very impactful, but of course, they didn’t believe me, so I had to demonstrate it. I went off for 7 days and then went in to my rheumatologist’s nurse practitioner. She saw my hands twisted, red and inflamed to three times the size of what is normal, and also observed the spasms in my back that also severely affected my breathing. I’m allergic to all NSAIDs including ibuprofin and naproxen sodium because of mast cell activation syndrome, so I’m not able to take anything besides Tylenol at this point, which is absolutely unhelpful. After seeing for herself, she agreed to continue the steroids. (Side note: the cardiologist told me that I obviously gained weight on the steroids because I was eating more. Wrong. I eat about 1,000-1,2000 calories a day. Doctors love to shame women. One of my fellow patients was told to lose weight when she only weighed 95 pounds at 5’4″.)
I went back in to Barrow to follow up on an EEG. I had reacted to the strobe light even though it hadn’t been noted on the report and the tech saw it happening and kept asking if I was okay. I also have been having issues with my tongue and mouth going numb, and my left arm has been having spasms. I know that my brain has had changes that are different from the last two MRIs. This appointment was set up with a nurse practitioner because the neurologist I previously had left Barrow (yes!!! he was horrible), so we had never met. It seemed like she understood what I was explaining about my history. She left the room, came back, and said, “We’re really specific here, and no one knows what to do with you. Can you just go to a neighborhood neurologist? Maybe they will know what to do with you.” Seriously. When I go to a neurologist who is outside of a big organization like Barrow, they throw up their hands and say, “But I’m just a neighborhood neurologist!! What do you want from me?” The NP gave me two names as a suggestion, but since I saw a different doctor in the same office already, I can’t see anyone else.
My thyroid stopped working at optimal, which explains why I was feeling extra tired and achy, and looking even more like a defensive tackle. Whenever that happens my cholesterol also goes through the roof. So I had to adjust all those meds again.
I’m being monitored for clotting by an oncologist/hematologist, so I had to go in for more tests. Right now it looks like my factor IV and fibrinogen are high. The fibrinogen makes sense because of what has happened to all of my shunts.
I need to have a laser treatment on my gums and one of my molars pulled but that has to be put off indefinitely because of the current situation. These are complications in my mouth because of mast cell activation syndrome. I can’t ever get dental implants, also because of mast cell activation syndrome – I’m allergic to metal, cement and glue/bonding.
Throughout all of this, I’m also trying to coordinate all of my meds. Some are traditional meds that I can get through a place like Walgreen’s. However, I’ve encountered some shortages. So it’s been left up to me to follow up to try to figure out how to get them. One of my meds I couldn’t get for FOUR months. Some of my medications have to be compounded because they aren’t available in the form I need to take them on the regular market. For instance, one is available as an eye drop, but I need to be able to take it as a pill. But the prescribing doctor is in Minnesota, and I’m overdue to see him, and he can’t do a televisit because I’m not physically in MN. None of my other doctors will write the script. See how this shit gets complicated? Besides that, I also had to go through the approval process multiple times for the shots because I failed out of multiple medications. I talked, I faxed, I talked some more, I faxed some more, I scanned, I talked, I waited on hold, I faxed, I scanned, I faxed…you get the idea. Oh, and they also ran credit checks on me. That’s something new all of them are doing. They are saying it’s because they want to make sure I’m getting all the benefits I can get, but obviously that’s a big fat lie. I’m wondering who they are withholding medication from. Drug manufacturers have a lot of power.
That sums up everything I have been dealing with for the past couple of months.
I’m on Social Security Disability Income (SSDI), which means I worked before I became disabled. In fact, the judge that decided my case said I truly worked as much as I possibly could before I really couldn’t work anymore. I now fall into the category of having a very low income, but it’s not low enough to receive any additional help. I don’t get any assistance with housing/rent, food, utilities or transportation. Some people get discounts but I don’t. The last time I had this income was 1993.
With this income, I have to pay for my monthly medical premiums. The premiums alone add up to $438.20. One of the plans I have isn’t from the state I live in. The state of Arizona doesn’t believe that someone could exist who is below the age of 65 and receives income above poverty level, who is also disabled. That’s me. They don’t have any policies for anyone under 65 who isn’t poverty. The craziest thing happened, though. I was actually living in another state when my case was decided, and the state had one – only ONE – policy that I could buy that could travel to any of the other 49 states no matter where I lived. I just can’t miss a payment for the next 22 years, ever. If I do it could mean hundreds of thousands of dollars of extra costs for me because of all of my crazy health stuff. This dollar amount does not include the money I spend on prescriptions, OTC meds or supplements. The supplements are absolutely necessary because they help to treat mast cell activation syndrome.
I spend something in the neighborhood of $100-150 on transportation a month because of having to go to doctor appointments, labs, scans and to the pharmacy. For about a month and a half Medicare was allowing our medications to be delivered, but they stopped allowing that, so I have to go and get my meds now. We can’t do mailing here in AZ because the heat degrades medications. (There have been a few times when the ice packs have been barely cold on my shots that have been delivered to me.)
I am signed up on two different transportation programs for disability, and I’m supposed to wait outside and be visible to the drivers. This is fucking hell in AZ in the summer. My heart condition makes it so much harder for me to be up and out in the heat.
So let’s talk masks, and COVID-19.
I have 8 masks now, with vents. My very first mask a few years ago was a Vogmask. I started wearing it on flights because I wanted to avoid breathing in the shit everyone was passing around in the cabin, because I was sure to catch whatever they were dishing out. So far it’s worked. And let me tell you, those vents make all the difference. Right now I’m on a list for the backordered masks from England for the fanciest of fancy vented Cambridge masks; I’m in for 2.
I’m up on COVID-19. I’m comfortable with the science, been correcting misinformation. One of my drivers tried to tell me the 19 stood for it being the 19th version of the virus. Ha. Ha. Nope. I think the people who walk around saying their freedom is being taken away are complete assholes and deserve what they get. I think the people who say they will make themselves sick with bronchitis or other lung infections by wearing a mask are assholes.
So when I’m going around to all of these appointments, seeing my doctors, getting labs and scans done, I have my mask on. There have been a few times where there blackness has been closing in on me because transportation has insisted I be outside in 100+ heat, my wig is dripping hot, I’m gasping for air, and I have to pull the mask off because I can tell my pulse is through the roof and my BP is dropping. It will happen at the grocery store too. I’ll be walking around and suddenly my body will just crash. I have to take the mask off for a few so I don’t end up on the floor. I do my best to stay masked up unless my body rebels. When the episode is done, the mask goes back on.
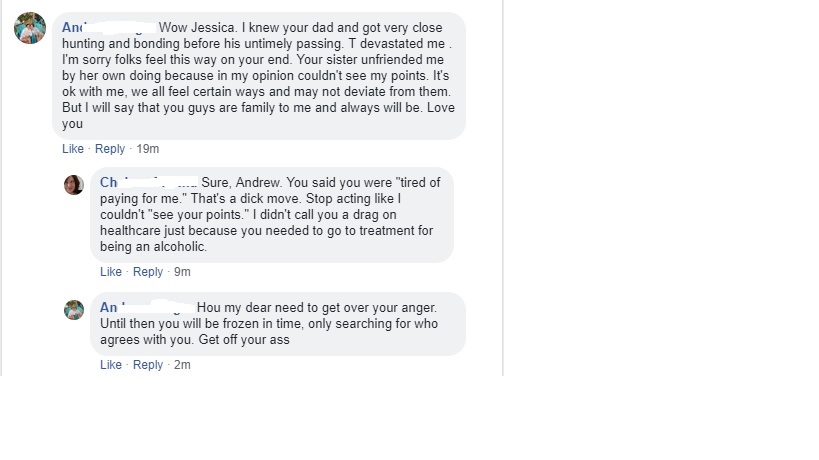
Last night, a friend posted on Facebook that if someone didn’t mask up, he was going to cut that person or people off (with an exception for some medical situations). I saw some people posting, including comments about how there was no way there should even be exceptions for medical. So I raised my hand and said hey wait a second, there has to be exceptions, and we still need to go out. And one guy lectured me about how I needed to have my groceries and prescriptions delivered and my doctor visits should be telemed. I told him to fuck off.
I don’t know this guy. He doesn’t know my shit. But groceries cost me at least $30 extra delivered because of the delivery fee and tip, and they NEVER get what I need and they never do substitutions when I ask for them, which would result in another run to the grocery store. Do I have tons of extra money to spend? Do I have $30, or $60, or $120 a month to throw away on delivery fees? Prescriptions were only allowed to be delivered by Medicare for a short amount of time. Now I have to go and get them again. As far as the doctor visits go, my shit is so complicated that I am required to go in. The docs don’t give me a choice.
This guy’s response was that he thought I would want to not spread the virus and be responsible, and if I didn’t wear a mask, I should just at least pull my shirt up over my mouth and nose. So I told him that I’m not a bottomless pit of wealth, and he’s telling someone who uses a cane and two arm braces and whose face is also partially paralyzed to walk and pull her shirt up. He then offered to “get my groceries” and I told him to stop talking. His response was “Damn.” A particularly dumb broad piped in about how rude I was to refuse his help by telling him to fuck off.
Being a disabled, middle-aged, single, adult female is a fucking challenge. There was that time when a complete stranger grabbed me by the arm and dragged me into an elevator because I was waiting for someone to turn around their power scooter and he assumed I couldn’t handle the elevator on my own. So here’s this guy on Facebook telling me that I have to pay for delivery and get only half of what I need, get my prescriptions delivered (even though Medicare doesn’t allow it) and just see my doctors on video (even though they won’t allow it). Yes, I’m going to tell him to fuck off. He offered to get my groceries AFTER I told him to fuck off. He wanted to feel better about being an asshole and making HUGE assumptions. I would never, ever, ever let someone near my groceries, my medications or my living space who would try to ridicule me like that and then try to strap on the hero cape. “No, really, I’m a good guy.” Don’t ever trust a guy who tells you he’s a good guy right after he does something shitty. And I’m still masking up.