Happy Holidays! Froeliche Weihnachten! Happy Hanukkah! Happy Kwanzaa!
What is Santa/Kris Kringle/Krampus/Monito-monita, that crazy, overgrown elf/Viking who has nothing to do with a mythical baby born in a stable bringing you this winter solstice/Christmas/yule?
I already got my gift, but nothing like what the three wise men brought across the desert. At the beginning of November I saw a new neurologist who agreed to give me everything that I seemed to be missing: an upright MRI, a neuro psych test, and keep me on as a patient, as confusing as my case is. Three days after our initial meeting the doctor who administers the neuro psych tests had a cancellation so I didn’t have to wait four months. A neuro psych test is a series of tasks to evaluate my real brain functionality – not just the few words a doctor might ask you to remember a few minutes later, like “pencil,” “dog,” and “purple.” I had to take many different kinds of timed tests, including drawing, making linear connections, making word associations, and answering personality questions. That’s the short version.
I didn’t have any problem with drawing pictures from memory. I was shown simple lines and boxes and then given a blank piece of paper a half hour later and could draw them in sequence perfectly. However, when it came to things like giving a list of words that began with a certain letter in the space of 60 seconds, it was like the bottom of my brain fell out. I could only give four words for the letter “A,” and they were very simple words like “an” and “apple.” There were four letters total, and each letter was a challenge. I can only remember the letter “A” at this point.
There was another exercise where the tester gave me a list of words that included pieces of furniture, animals, and modes of transportation. Every time I repeated the list back, I always tried to give it back in order, I never tried to group everything together in like groups. It never occurred to me. However, if I had full functionality, it probably would have. I also could never remember more than a few words, even though I’m guessing the list was repeated more than 20 times.
They wanted to see how I could do with repeating numbers back, so they started with three numbers, then four, then five. As soon as I got to five, I started struggling. At six, I couldn’t repeat any numbers, not even the last two or three of the group. Again, it was like the bottom of my brain dropped out.
There were many other tests, but in the interest of space and to save some face, I’ll stop there. You get the idea.
A few weeks later when I could meet with the doctor who administered the test, she confirmed what I dreaded hearing but suspected: I have brain damage. Since I’ve never had an evaluation done before there’s nothing to compare it to, but she said she could tell that in some areas my knowledge base and functionality was “superior,” or above the level of a college-educated woman. However, the brain damage affected my memory and speed and speech and brought those areas down to true mental impairment.
A few days ago I went into the office for part II of my follow-up to look at the actual scans of my upright MRI. My MRI did not look good.
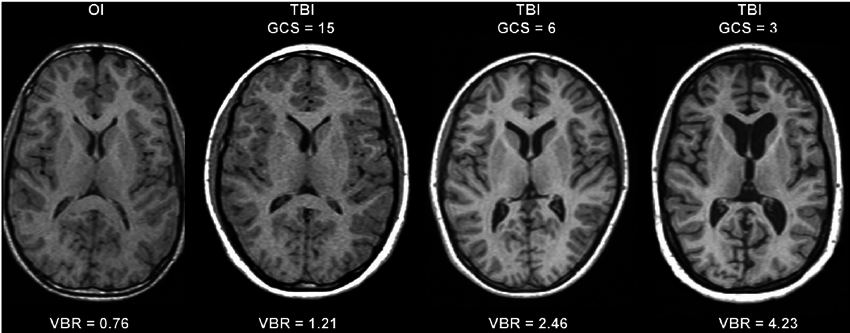
Above is a progressive MRI scan of a brain (not mine), moving down from top to bottom. As you move further down, you notice that the part in the middle gets larger and darker; that’s the ventricles. They are the four chambers that are the gold standard for figuring out if there’s a problem with CSF in the brain. This is what normal looks like.
Unfortunately, I don’t have any ventricles left. All of them have collapsed. My brain is pressing on the brain stem and I’m having all kinds of unusual problems, like my legs suddenly jerking if I’m standing and I look down briefly. Of course I have the problems I’ve always had, like the vertigo and the fatigue, and that pesky facial droop and ptosis (pronounced “toe-sis”). My new neurologist insisted that the disappearance of my ventricles must mean that I’m overdraining, but I knew that I must be suffering from Slit Ventricle Syndrome, and it means just the opposite – the pressure is crushing my brain.
UCLA has a pretty good explanation of Slit Ventricle Syndrome. I’m 100% certain that my shunt is “nearly blocked but barely flowing.” I always, always feel like my intracranial pressure is extremely high. It’s exhausting. So for now, it looks like I have Slit Ventricle Syndrome, and I’m not sure if this would have been picked up before this point – at least not two or three years ago, even though the symptoms are the same. I don’t recall that my ventricles have looked this horrific in all of my 20+ prior MRIs.
Also troubling is trouble brewing at the back of my skull. In 2013 I had two cisternoperitoneal shunts placed when my neurosurgeon was trying to find anything, anything, that my body wouldn’t reject. After we removed those and I ended up with a ventriculoperitoneal shunt, he barely got the old one out after a lot of scraping and pulling because of the scar tissue that had built up along the tract. A surgery that should have been an hour and a half turned into five hours and I was left with a huge highway of bruising from my head to my abdomen.
Unfortunately, he thought that it wasn’t detrimental to leave scar tissue in my head, and in fact may help to plug the burr hole where he drilled for surgery so I wouldn’t have any leaks. I knew what it was like to have a CSF leak; 2014 was incredibly painful when I had a leaking shunt for that whole year. The scar tissue has been increasing in diameter and it’s now growing like a tumor. From what I can tell it’s about the size of a quarter, and it’s pressing on the area of the brain that deals with memory and speech. It’s actually a long rope but it’s got a huge bulb, and if I press on the burr hole, it yanks on the area it’s attached to right behind my ear.
In plain English: My brain is being crushed. My shunt isn’t working. I’m growing my own tumor that was started by my scar tissue.
My challenge is that I’m allergic to the shunt materials. Also, now that the scar tissue is turning into a growing tumor, can we take it out without creating a leak, and when we pull it out, will the area it’s damaging have permanent damage or will it heal?
Also, can I fucking qualify for disability now? Everything that I’m reading about Slit Ventricle Syndrome says that it’s a permanent condition – there’s no going back.
Within the next few weeks (because of the holidays messing everything up) I’ll find out when I can get in with the best neurosurgeon in the Minneapolis/St. Paul area. He came highly recommended by other hydrocephalus patients when I attended the hydrocephalus conference including the mother of Olivia, the young woman who had 123 surgeries since birth and who is now aged 20.
I am also in the process of finding an occupational therapist for an evaluation that can be included in my records for my attorney and disability case.
I’m going to share the most personal thing I possibly can and have up to this point, because some of you may doubt how much this has affected me because I have created coping mechanisms. It has taken me two full days to write this post and writing even the simplest words is sometimes a struggle. But the hardest thing for me to do to date was to send out holiday cards. At one point I had to stop writing for about a half hour because I broke down in tears. Hand writing words without the benefit of being able to go back and erase them and rewrite them like I do in the computer almost caused me a panic attack because I could no longer remember how to write even single-syllable words. For the people who did get cards, there was a lot more crossing out and scribbling than I would have liked. Maybe you noticed that I started to write an “E” where there should have been an “L” first. Sometimes I couldn’t even remember how to write my own name correctly – I would skip letters.
I don’t have all of the answers. I still – STILL – don’t know what’s causing the imbalance with the CSF in my brain. I don’t know if taking out the scar tissue/tumor is going to alleviate the memory and speed problems. I don’t know if I’m ever going to be able to tolerate an appliance in my body. I definitely don’t want to hear, “But you look fine!” or “Have you tried _____?”
.

